Related Articles
 Jan 08, 2025
Jan 08, 2025
Is Varicose Vein surgery covered under the health insurance policy in India
 Health Insurance
Health Insurance

It is said that the real worth of health insurance is understood during its claim. Considering the steep inflation in the healthcare sector, having a reliable, comprehensive health insurance plan has become mandatory. Without it, even a couple of days of hospitalisation is enough to affect your hard-earned savings significantly, especially when any surgery is involved.

When you possess a health insurance plan, you can settle your claim either through the cashless process or the reimbursement process.
In this sort of claim settlement, you receive quality treatment at any listed network hospital or healthcare facility without incurring any immediate out-of-pocket expenses. Here, the insurance company directly settles the bills with the hospital authorities as per the terms of the chosen plan concerned.
You simply need to get admitted to any of the network hospitals and present your insurance health card, where all the policy details are mentioned along with your identity proof.
However, you need to acquire your insurer’s approval before 72 hours in the case of planned hospitalisation. But, in the case of an emergency, you need to contact them at the earliest after hospitalisation within 24 hours.
Once the treatment is complete, you have to submit the claim form to your TPA (third-party administrator) or the insurance desk at the hospital, who is the liaison between you and your insurer. From here, your insurer takes up the case and proceeds.
The "Cashless Everywhere" policy allows insured individuals to avail cashless treatment at any hospital, even if it's outside the insurer’s network. This initiative aims to simplify hospitalisation by eliminating the need for upfront payments and reimbursement claims.
The initiative by the General Insurance Council (GIC) aims to make hospital treatments completely cashless across 40,000+ hospitals, benefiting over 30 crore insured individuals. It eliminates upfront payments, allowing insurers to settle bills directly with hospitals, reducing financial stress for patients.
While promising, challenges remain—many hospitals hesitate to join due to payment delays and complex authorisation processes. The system is still rolling out, so initial hurdles are expected, but it has the potential to increase trust, reduce fraud, and make healthcare more accessible in the long run.
In this case, your choice of hospital does not follow the list of network hospitals maintained by your chosen insurer. This means that you can receive treatment from any non-network hospital and settle the necessary dues by yourself. After discharge, contact your insurer for a reimbursement claim by submitting all the relevant documents along with the claim application form.
Here, you must submit all the documents, invoices, bills, invoices, reports, prescriptions, etc., rendered during the entire treatment procedure. The insurer reviews all these documents and may demand any additional documents if necessary. Once everything is reviewed to be right, the insurer settles the claim and transfers the approved amount to the registered bank account.
| Points Of Difference | Cashless Claim | Reimbursement Claim |
| Definition | This involves visiting any network hospital, where the insurance provider directly ensures the claim settlement. | Here, you need to bear the upfront treatment costs during discharge from the hospital and then present all the relevant documents for reimbursement claim approval. |
| Claim Process | The insured individual is required to inform the insurer beforehand and then file for claim settlement, which, in turn, directly settles the hospital bills. | The insured individual is required to clear the upfront hospital dues and then apply for post-treatment reimbursement after presenting all the relevant documents with the claim application form. |
| Claim Settlement | The insurer directly settles all the claims with the hospital authorities, considering the parameters of the chosen health insurance plan. | Here, the insured person needs to settle the dues first and then apply for claim settlement through reimbursement. |
| Claim Approval | You need to seek approval from your insurer 72 hours before any planned hospitalisation. In the case of an emergency, you have to contact your insurer within 24 hours of hospitalisation. | No claim approval is necessary. |
| Time Taken | Usually, it is comparatively faster than reimbursement claims. | Usually, it is more time-consuming than cashless health insurance plans. |
| Documents Needed | You need to duly fill in and sign the claim form offered by the TPA present at the network hospital. You have to submit all the relevant documents. | You have to submit all the invoices, prescriptions, reports, bills, receipts, etc. incurred during the treatment process. |
| Flexibility | The insured individual must opt for the treatment at a hospital within a network hospital. | You can avail of treatment from any of your chosen non-network hospitals. Claim reimbursement requires verification of the treatment procedure. |
| Hospital Availability | Exclusively available under the listed network of hospitals maintained by the insurer. | You can avail of treatment at any of your chosen non-network hospitals, maintaining the scope of your chosen plan. |
Considering the Indian scenario, in-patient hospitalisation proves to be expensive, irrespective of the type of treatment. Even if half a week of hospitalisation is involved, it depletes a significant portion of your savings.
Considering all these aspects, opting for cashless health insurance plans seems to be a better option. You need not have to worry about finances upfront. It will be taken care of automatically by your insurer, considering all the terms and conditions of your chosen plan.
However, if you need emergency hospitalisation, you can opt for any chosen non-network hospital. Under such circumstances, you can claim for a post-treatment reimbursement claim. But, here, you have to settle the hospital dues immediately after discharge.

Paybima Team
Paybima is an Indian insurance aggregator on a mission to make insurance simple for people. Paybima is the Digital arm of the already established and trusted Mahindra Insurance Brokers Ltd., a reputed name in the insurance broking industry with 17 years of experience. Paybima promises you the easy-to-access online platform to buy insurance policies, and also extend their unrelented assistance with all your policy related queries and services.
.png)
When you're planning to take a personal loan, knowing your monthly EMI in advance can help you stay financially prepared. The Muthoot Personal Loan EMI Calculator is a simple and efficient tool that provides instant EMI estimates based on your loan amount, interest rate, and tenure.


Relocating your two-wheeler to a different state needs to follow many procedures. Depending on the duration for which you are moving to the new place, it becomes necessary to transfer your vehicle papers if it is for more than a year. Although tedious, the process of relocating vehicles can become easy if you follow certain tips mentioned in this post. Read on!

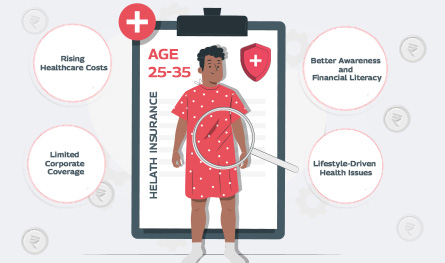
In what’s being called a quiet healthcare revolution, India’s young working professionals are reportedly making the most health insurance claims – outpacing even senior citizens. Surprised? So are the insurance providers. Young adults ranging between 25 and 35 years, who are often assumed to be in peak health, are now dominating the charts in health insurance claims by age.


If you think lifestyle-related health issues only show up after 40, think again. Youth no longer guarantees immunity. Today’s 25 - 35 age group is increasingly facing medical issues that only plague older adults. The reason? Long working hours at the desk, deliveries on speed dial, and a social life that rarely includes a decent amount of sleep are some of the reasons for the early onset of medical conditions like diabetes, anxiety, and hypertension.
