Related Articles
 Jan 08, 2025
Jan 08, 2025
Is Varicose Vein surgery covered under the health insurance policy in India
 Health Insurance
Health Insurance

Just having a health insurance plan does not suffice, you need to know the minutest details of your policy to take the maximum advantage of it. One such crucial benefit is the cashless claim facility that all health insurers provide. This offer allows policyholders to receive admission and treatments without any upfront payment to hospitals. The strength of the insurance company’s empanelled hospital network can impact your ease and convenience of treatments considerably.

It is said that “Life Happens”. In today’s hectic world, it is a luxury to dream of a completely healthy life with no unwanted surprises. It can be an accident, a sudden ill health or even a pandemic that can dig deep into your savings. To face such emergencies with confidence, a cashless scheme is a welcome step in any health insurance plan.
If you opt for a cashless scheme, your medical bills, treatment expenses and pharmacy bills will be directly settled by your insurer with the network hospital without your intervention. It means you can focus on recovery, and the monetary end is taken care of by the plan. It is extremely helpful at times when you are the one carrying the financial burden of your family and need to be hospitalised. Family members might not be in a position to arrange funds overnight for admission, treatment or even surgery. A cashless arrangement of the insurer with the empanelled hospital becomes a blessing which brings much relief to your family.
Health insurance companies have direct tie-ups with hospitals all over India. These partnered hospitals are called network hospitals. They are selected after an extensive check on the background and medical services, amenities, tariffs and quality of staff possessed by the hospitals. These tie-ups are on a renewal basis and are renewed annually after a detailed review of its services. This establishes the credibility of the insurer as well. This list is shared by the insurance company with the policyholders at the onset of the policy.
The company’s representative or Third Party Administrator (TPA) usually takes care of all the formalities. This TPA acts as a coordinator between you and the insurance company. It is responsible for making your claim settlement seamless, but it has the authority to deny your claims as well.
The documents that are essential for cashless claim processing are :
Follow these 5 simple steps to get your cashless claim :
To make your cashless claim experience even smoother, inform your insurer at the earliest whether planned or unplanned hospitalisation, give detailed and correct information about the patient’s medical history and pre-existing conditions and check for the inclusions and exclusions in your policy to avoid any surprises.
Here is a list of empanelled hospitals for some of the top insurers in the health insurance market:
Top Insurers |
Hospital Networks |
Bajaj Allianz Health Insurance |
Over 8,000 |
More than 22,900 |
|
HDFC Ergo Health Insurance |
Above 12,000 |
Niva Bupa Health Insurance |
9,100 |
Over 7500 |
Since the process of cashless claims in health insurance plans heavily depends on the quality of service of the insurer and its empanelled hospitals, the first step to avail of this benefit involves choosing the right insurance company. Remember, it not only takes away the financial stress but also can give you access to the best of hospitals with the best of doctors and advanced facilities which is so crucial in medical treatments. Some checkboxes that need to be ticked are :

Paybima Team
Paybima is an Indian insurance aggregator on a mission to make insurance simple for people. Paybima is the Digital arm of the already established and trusted Mahindra Insurance Brokers Ltd., a reputed name in the insurance broking industry with 17 years of experience. Paybima promises you the easy-to-access online platform to buy insurance policies, and also extend their unrelented assistance with all your policy related queries and services.
.png)
When you're planning to take a personal loan, knowing your monthly EMI in advance can help you stay financially prepared. The Muthoot Personal Loan EMI Calculator is a simple and efficient tool that provides instant EMI estimates based on your loan amount, interest rate, and tenure.


Relocating your two-wheeler to a different state needs to follow many procedures. Depending on the duration for which you are moving to the new place, it becomes necessary to transfer your vehicle papers if it is for more than a year. Although tedious, the process of relocating vehicles can become easy if you follow certain tips mentioned in this post. Read on!

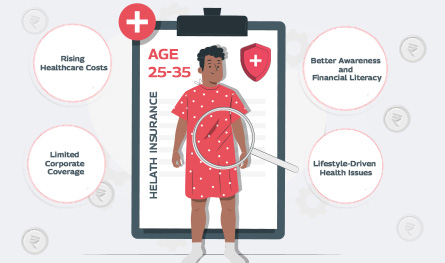
In what’s being called a quiet healthcare revolution, India’s young working professionals are reportedly making the most health insurance claims – outpacing even senior citizens. Surprised? So are the insurance providers. Young adults ranging between 25 and 35 years, who are often assumed to be in peak health, are now dominating the charts in health insurance claims by age.


If you think lifestyle-related health issues only show up after 40, think again. Youth no longer guarantees immunity. Today’s 25 - 35 age group is increasingly facing medical issues that only plague older adults. The reason? Long working hours at the desk, deliveries on speed dial, and a social life that rarely includes a decent amount of sleep are some of the reasons for the early onset of medical conditions like diabetes, anxiety, and hypertension.
