Related Articles
 Jan 08, 2025
Jan 08, 2025
Is Varicose Vein surgery covered under the health insurance policy in India
 Health Insurance
Health Insurance
Do you know that you can lodge a complaint against your Health Insurance Company if you are unhappy or dissatisfied with their services? In this post we will read the guidelines to follow to complete the procedure.
When we buy a health insurance policy from a health insurance company, we expect some services and benefits from the insurer as mentioned in the policy papers. However, if we do not receive the facilities as promised, we become unsatisfied with the policy provider. If you feel that you are not satisfied with your insurance company, you can approach the IRDAI or Insurance Regulatory and Development Authority of India to find a solution. You can escalate the issue in various ways by means of an IRDA complaint.
There is a certain Turn Around Time (TAT) that the IRDAI has allowed for different services provided by insurance providers. As per rule, the turnaround for life insurance and general insurance is maximum depending on the kind of issue or grievance that is required to be addressed. If the insurer does not comply with the TAT to resolve a particular issue, the policyholder can seek interference by the IRDAI to resolve the same. However, if the policyholder escalates the dispute to IRDAI, the association is required to resolve it with the insurer. Further, if any enquiry is needed regarding the issue, the insured can move towards the consumer court.
Below is the process to lodge a Complaint against a Health Insurance Company:
Below are the steps:
If you want to lodge a complaint with the IRDAI against your insurer, you must contact the IRDAI’s Grievance Redressal Cell. This cell is a part of the Consumer Affairs Department of the association and one can submit the complaint via IRDA Complaint mail id or calling the customer services. IRDAI offers an Integrated System of Grievance Management that monitors the complaint after it is lodged. The insured can get in touch with the association via mail or fax.
Below is the maximum TAT for particular grievances associated to certain services of the health insurers:
| Particular Services | Maximum TAT |
| Proposal Processing & issue or cancellation of a plan | 15 days |
| getting the proposal copy of the policy | 30 days |
| Grievances related to errors/refund/NCB etc. | 10 days |
| Grievances pertaining to Surrender value and Annuity | 10 days |
| Requests related to maturity claim, survival benefit or non-payment of penal interest | 15 days |
| Concerning claim raising requirements once a claim is registered | 15 days |
| For settling death claim without the requirement of investigation | 30 days |
| For death claim denial or settlement that needed investigation | 6 months |
| Admitting a grievance | 3 days |
| Grievance resolution | 15 days |
Hence, to initiate the process you need to contact the helpdesk of your insurer to resolve your issue. In case the TAT is over and the issue still persists, you may escalate the problem to IRDAI.
Here are the contact details of the top health insurance companies’ Grievance Cell:
| Insurance Company | Email Address |
| Care Health Insurance | customerfirst@carehealthinsurance.com |
| Bharti AXA Health Insurance | customer.service@bharti-axagi.co.in |
| Bajaj Allianz Health Insurance | customercare@bajajallianz.co.in |
| Apollo Munich Health Insurance | customerservice@apollomunichinsurance.com |
| Cholamandalam MS General Insurance | customercare@cholams.murugappa.com |
| IFFCO Tokio Health Insurance | websupport@iffcotokio.co.in |
| HDFC Ergo Health Insurance | care@hdfcergo.com |
| Max Bupa Health Insurance | customerfirst@maxbupa.com |
| ICICI Lombard Health Insurance | grievance@icicilombard.com |
| Future Generali Health Insurance | care@futuregenerali.in |
Contact Details for Grievance Redressal Cell of the Consumer Affairs Department for IRDA complaint:
| Toll Free No. | 1800 4254 732/ 155255 |
| IRDA Complaint E-mail ID | complaints@irda.gov.in |
| Postal Address | Consumer Affairs Department Insurance Regulatory and Development Authority, 3-5-817/818, 9th Floor, United India Towers, Hyderguda, Basheerbagh Hyderabad – 500 029 |
| Fax | 040-66789768 |
You can lodge a complaint against your insurance provider via three main channels – the Insurance Ombudsman, the Integrated Grievance Management System and the Consumer Court.
Insurance Ombudsman is the first channel in case you want to escalate an issue pending with your insurance provider.
Following are the conditions to file a complaint with the Insurance Ombudsman channel:
This is an online channel introduced by IRDAI. Here, the policyholder who wants to lodge a complaint against the insurer may escalate the issue. This system allows the complainant to register and track the progress of the complaint online.
Further, this system offers a unique ID to the complaints and dispenses them to the particular departments to get resolved. This way monitoring the complaint becomes easy and also ensures efficient resolution of the issue in a proper system.
Lastly, if the issue persists and is unresolved, the complainant can move to consumer court, which handles grievances related to health insurance separately. You can submit your complaint at the consumer forum complaint email id.

Paybima Team
Paybima is an Indian insurance aggregator on a mission to make insurance simple for people. Paybima is the Digital arm of the already established and trusted Mahindra Insurance Brokers Ltd., a reputed name in the insurance broking industry with 17 years of experience. Paybima promises you the easy-to-access online platform to buy insurance policies, and also extend their unrelented assistance with all your policy related queries and services.
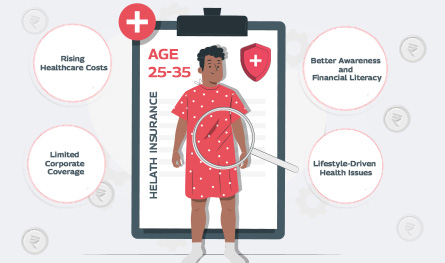
In what’s being called a quiet healthcare revolution, India’s young working professionals are reportedly making the most health insurance claims – outpacing even senior citizens. Surprised? So are the insurance providers. Young adults ranging between 25 and 35 years, who are often assumed to be in peak health, are now dominating the charts in health insurance claims by age.


If you think lifestyle-related health issues only show up after 40, think again. Youth no longer guarantees immunity. Today’s 25 - 35 age group is increasingly facing medical issues that only plague older adults. The reason? Long working hours at the desk, deliveries on speed dial, and a social life that rarely includes a decent amount of sleep are some of the reasons for the early onset of medical conditions like diabetes, anxiety, and hypertension.


Remember when a simple doctor’s visit felt like planning a mini-event? First, you had to book an appointment days ahead, then sit in a crowded waiting room, scrolling aimlessly while watching the clock tick past your slot. It's not exactly the highlight of anyone’s week. Well, those days are pretty much over. Enter telemedicine – the futuristic healthcare option that is slowly becoming the cornerstone of modern medical insurance plans. From coughs to consultations, you can now connect with a doctor from your living room or your office—or even mid-binge on your favourite series. It’s healthcare that works around your schedule, not the other way around.


Have you noticed how your routine visits to your doctor or a basic diagnostic test feel more expensive every year? Well, you’re not imagining it. Healthcare costs are rising faster than ever before, and unlike general inflation that affects groceries and fuel, medical inflation hits harder because it generally strikes during emergencies.


If you ever feel like your health insurance premium is slowly eating up a sizeable chunk of your pay stub every year, you are definitely not alone. With the rising costs of medical procedures and insurance companies adjusting to increasing claims and inflation, even basic health insurance coverage can start to feel like a financial burden.
