Related Articles
 Jan 08, 2025
Jan 08, 2025
Is Varicose Vein surgery covered under the health insurance policy in India
 Health Insurance
Health Insurance

The process of health insurance claims can leave the most seasoned healthcare consumers baffled and helpless. Thus a clear understanding of the entire claim process is of importance both for your financial health and mental peace. Once you know the timelines and the methods to navigate the complex path, these daunting tasks become a cakewalk, even in a stressful situation.
Who would like to be harassed about a claim process which is ideally supposed to support you financially? You would surely prefer to focus completely on recovery from illness rather than any bureaucracy and complicated paperwork.

The basic steps of insurance claim settlement involve the following:
The settlement process begins only when you inform your insurance provider about your admission into the hospital or the beginning of any treatment, be it planned or under emergency.
Pro tip: Emergency claims must be intimated to the insurer within 24 hours of hospitalisation, while planned claims need prior approval at least 3-4 days before hospitalisation.
Even if you do not wish to file a cashless claim, it is prudent to keep your insurer informed.
The insurance company will ask for certain documents either during the treatment or after it, including hospital bills, medication prescriptions, pharmacy bills etc. to asses the requirement.
For cashless claims, your hospital will liaise with the insurer on your behalf and provide all the original documents for the claim settlement process.
However, for Reimbursement Claims, you must submit all the original documents to the insurer, along with a duly filled and signed claim form and your bank account details for the claim to be processed.
To evaluate the authenticity of your claim, the insurance provider will verify all documents and information you provided.
Pro tip: Adjudication of claims refers to the process by which your provider decides whether to settle or reject your claims based on your policy terms and conditions.
The company decides after thoroughly reviewing your situation and condition and prior claim history. If the claim is approved, the funds are directly paid to your hospital in Cashless Claims or reimbursed to you after subtracting any deductibles or co-payments in Reimbursement Claims.
STEPS OF THE CLAIM PROCESS |
TYPES OF HEALTH INSURANCE CLAIMS |
||
|
Cashless Claims: Only applicable if admitted to network hospitals of the insurer. |
Reimbursement Claims: If you need to admit your patient to non-empanelled hospitals or if the cashless process is delayed by the hospital, the reimbursement process is followed. |
|
Cashless Planned Hospitalisation |
Cashless Emergency Hospitalisation |
|
|
Step 1 |
3-4 days before hospitalisation, a cashless claim form is to be submitted to the insurer via letter or email. |
The insurance provider is to be notified within 24 hours of hospitalisation. A claim intimation number is then generated and shared with you |
The insurance company should be intimated via email or call within 2 days of hospital admission. |
Step 2 |
Once the form is received, the insurance company will inform the hospital |
The claim insurance form needs to be filled out by the hospital with all details and submitted to the insurer. |
The claim form from the insurer’s website needs to be downloaded and filled. |
Step 3 |
The insurer will send you a confirmation letter with a validity of 7 days from the date of issue. |
The insurance provider sends an authorisation post-receipt of your claim form. |
Several documents like discharge summaries, doctor’s bills, test reports, and in-patient records are to be submitted along with parts A and B of claim forms. |
Step 4 |
The confirmation letter and your health card will be submitted to the hospital to enjoy the cashless benefits. |
The expenses incurred are cleared by your insurer directly with the hospital. In case of claim rejection, you will be notified by email or via message. |
The insurance company or the Third-Party Administrators (TPA) will check in detail all documents submitted and if approved, settle the claim via bank transfer with a TAT of 10-15 working days. |
Along with the claim form, these documents are critical to be submitted for claim clearance :
However, there may be delays even after submitting all things required. To reduce insurance claim delays and rejections, certain checks are needed to be done at your end :
To reduce delays for such reasons and to streamline the operation, a Third Party Administrator (TPA) is brought in to ease out the insurance claim process in the following ways :

Paybima Team
Paybima is an Indian insurance aggregator on a mission to make insurance simple for people. Paybima is the Digital arm of the already established and trusted Mahindra Insurance Brokers Ltd., a reputed name in the insurance broking industry with 17 years of experience. Paybima promises you the easy-to-access online platform to buy insurance policies, and also extend their unrelented assistance with all your policy related queries and services.

Relocating your two-wheeler to a different state needs to follow many procedures. Depending on the duration for which you are moving to the new place, it becomes necessary to transfer your vehicle papers if it is for more than a year. Although tedious, the process of relocating vehicles can become easy if you follow certain tips mentioned in this post. Read on!

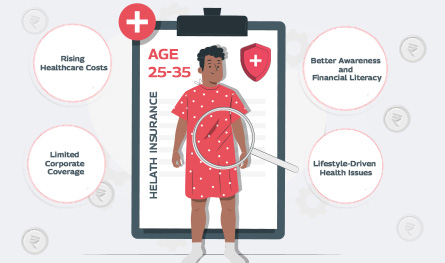
In what’s being called a quiet healthcare revolution, India’s young working professionals are reportedly making the most health insurance claims – outpacing even senior citizens. Surprised? So are the insurance providers. Young adults ranging between 25 and 35 years, who are often assumed to be in peak health, are now dominating the charts in health insurance claims by age.


If you think lifestyle-related health issues only show up after 40, think again. Youth no longer guarantees immunity. Today’s 25 - 35 age group is increasingly facing medical issues that only plague older adults. The reason? Long working hours at the desk, deliveries on speed dial, and a social life that rarely includes a decent amount of sleep are some of the reasons for the early onset of medical conditions like diabetes, anxiety, and hypertension.


Remember when a simple doctor’s visit felt like planning a mini-event? First, you had to book an appointment days ahead, then sit in a crowded waiting room, scrolling aimlessly while watching the clock tick past your slot. It's not exactly the highlight of anyone’s week. Well, those days are pretty much over. Enter telemedicine – the futuristic healthcare option that is slowly becoming the cornerstone of modern medical insurance plans. From coughs to consultations, you can now connect with a doctor from your living room or your office—or even mid-binge on your favourite series. It’s healthcare that works around your schedule, not the other way around.
