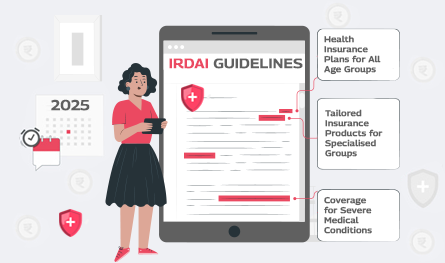
1. Health Insurance Plans for All Age Groups
As part of the recent policy changes, health insurance products no longer impose age restrictions. Previously, policies were restricted to people under 65 years old. Now, health insurance companies must provide at least one policy, accepting applicants regardless of age. The modified policy enables elderly individuals to obtain essential health coverage at any stage of their lives.
2. Shorter Waiting Period for Pre-existing Conditions
The traditional waiting time for people with diabetes or high blood pressure was established at four years. The new guidelines have reduced this time to three years. Thus, people with long-lasting health conditions now obtain financial treatment support in a shorter period, improving their healthcare timing and affordability.
3. Standardised Waiting Period for Specific Treatments
Through these reforms, the waiting times for specific medical procedures have become standardised. Joint replacement surgeries require patients to wait three years according to the standardised treatment period. The standardised waiting periods enable patients to prepare their medical needs better while ensuring clarity concerning the claim benefit timeline.
4. Coverage for Severe Medical Conditions
The updated standards prohibit Insurers from denying coverage benefits to patients for severe illnesses. According to the new rules, people who are diagnosed with severe heart disease, cancer, or kidney problems cannot be denied coverage automatically. The system now provides equal opportunities to all people through specific terms and waiting periods which remain applicable.
5. Full Coverage for AYUSH Treatments
The guidelines have adopted a policy to provide complete coverage for AYUSH treatments which include the practices of Ayurveda, Yoga, Naturopathy, Unani, Siddha and Homoeopathy without any coverage restrictions. Policyholders receive complete reimbursement for their treatments from the insured amount without any coverage limits when availing AYUSH or modern healthcare services.
6. Tailored Insurance Products for Specialised Groups
The insurance industry receives encouragement to develop specific insurance plans catering to distinct community groups. The new guidelines require insurers to develop specific insurance plans targeting children, senior students, and expectant mothers. Customised health policies address the distinct requirements of different population groups to help individuals select coverage that meets their specific health needs.
The new regulations demand that health insurers establish networks of hospitals which support cashless claim payments. Policyholders can benefit from this feature as their healthcare providers will receive direct payments from insurers at network hospitals, eliminating immediate payment concerns.
8. Reduced Moratorium Period
Previously insurers were allowed to challenge claims based on undisclosed information for extensive periods. The new insurance regulations reduce the time insurers can contest claims from seven to five years [unless fraud can be proven through definite evidence]. The modification enhances confidence between insurance companies and policyholders.
9. Model Products for Vulnerable Sections
The insurance sector now requires insurers to develop model products that specifically benefit vulnerable groups. People with disabilities and chronic illnesses fall under this category. The new guidelines feature policies in favour of these groups to provide necessary healthcare coverage for every individual.
10. Multiple Claims Across Insurers
The reforms enable policyholders holding benefit-based plans to submit their claims to multiple insurance providers. Healthcare recipients benefit from this adaptability as avail maximum coverage protection while receiving optimal medical assistance.
.png)